Key Components of a Leading Bariatric and Metabolic Surgery Centre
Rising Incidence of Morbid Obesity
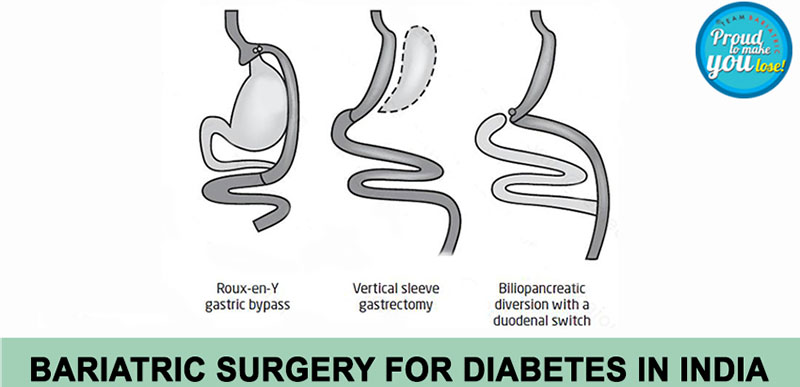
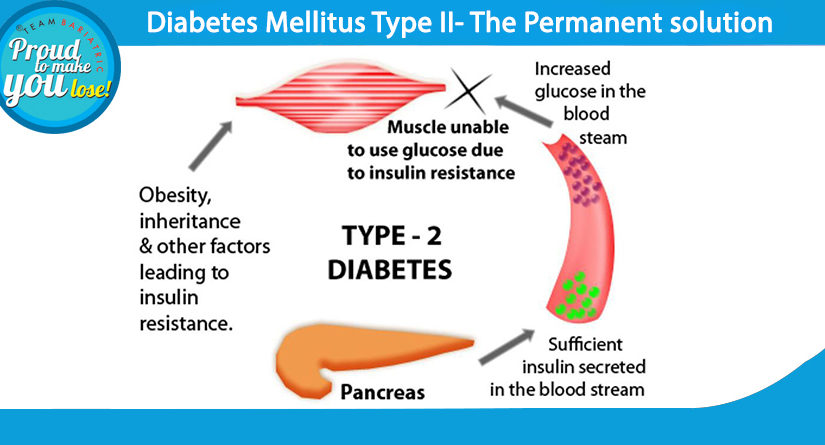
As the incidence of Morbid Obesity is rising day by day, more and more hospitals have started bariatric surgery programs. However, managing a morbidly obese patient is challenging in the way that obesity brings a lot more other diseases with it. Obstructive sleep apnea, Diabetes Mellitus type 2, Hypertension, and Hypothyroidism are a few of them.
Therefore it’s mandatory to set up a comprehensive management program for treating these patients in the best bariatric and metabolic surgery centre.
The decision to recommend bariatric surgery requires a multidisciplinary approach to evaluate the indications for surgery and to define co-morbidities properly.
Key Components of a Bariatric and Metabolic Surgery Centre
The surgeons at the best bariatric hospital must demonstrate the necessary training skills, experience, and leadership. The essential components of a bariatric surgical center include a Director, critical support, appropriate equipment and instruments, 24-hour qualified call coverage, continuous care, long-term follow-up care, and most importantly regular support groups. There must be facilities for data collection and maintaining a database. By collecting and sorting data, a well-maintained database would demonstrate past performance and help in directing future trends. Periodic evaluation and comparison will allow centers to develop improvement plans.
Role of the Bariatric and Metabolic Committee
There must be a bariatric and metabolic committee which is headed by the program director and includes the coordinator, clinical reviewer, and hospital administration staff. All the surgeons included in the committee must focus on quality improvement which includes a reduction in variation, standardization of practice, establishing selection guidelines, and quality improvements. This can result in decreasing rates of complications, re-admissions, length of stays, surgical site infections, etc. The committee also establishes pathways of care for pre-operative and post-operative management. All relevant staff must be educated in patient safety and complication recognition. The goal of the pathways is to prevent failure to rescue situations which means early recognition and treatment of the post-surgical complications.
Responsibilities of the Bariatric Surgical Care Coordinator
The Bariatric Surgical Care coordinator assists and reports to the director of the committee. The coordinator assists in center development, managing the accreditation process, maintaining relevant policies and procedures, patient education, outcomes and data collection, quality improvement efforts, and education of relevant institution staff. The coordinator supports the development of written protocols and education of nurses to recognize the critical vital signs required to minimize delays in the diagnosis of serious adverse events.
Data Management and Accreditation
The clinical reviewer enters data into relevant platforms. The reviewer should not be contributing to patient care to avoid bias.
The hospital must be accredited by relevant authorities to ensure that the care for metabolic and bariatric surgery patients is provided in a safe environment. In this respect, Apollo Hospitals New Delhi has been accredited by the JCI.
Certifications and Training
The director or the chief surgeon must have obtained a verification certificate to operate on morbidly obese patients by relevant governing bodies. These certificates are purely based on the volume of surgeries and quality of care and dedication to the practice. Similarly, there must be 24-hour call coverage for the patients attended by qualified persons.
The bariatric surgical nurse must obtain specialized training such as the Certified Bariatric Nurse certification.
Essential Support Services
There must be dedicated physicians, dieticians, psychologists and psychiatrists, social workers, and physical therapists.
Registered dieticians are absolutely essential for the success of any bariatric surgical center.
They do all the nutritional counseling and follow-up.
Psychologist and psychological evaluation is a must before any bariatric and metabolic procedure. These patients are often suffering from depression, anxiety, and other stress-related disorders. Psychological education, evaluation, and preparation are useful in achieving overall patient stability and emotional well-being.
Facilities and Equipment
Morbidly obese patients must feel welcome upon entering an institution. There must be appropriate furniture to accommodate them in the waiting room as well as the examination room. The plus size hospital clothes, beds wheelchairs, and floor-mounted toilets are a must. There must be dedicated beds or floors for bariatric surgical patients. Similarly, operating room tables and equipment are accordingly sized to the needs of such patients.
Critical Care and Anesthesia
The critical care support providers must be trained in identifying early signs of potential complications. The anesthesia team must be trained to give anesthesia to such patients taking care of DVT prevention and obstructive sleep apnea to name a few.
Various specialty consultants are also asked to give preoperative clearances to the patient in view of the existing co-morbid conditions.
Support Groups and Electronic Media
A pediatric and adolescent medical advisor is also a part of the team at the center. He/she operates on adolescent patients.
Support groups are designed for the patients who are in the recovery phase. These are primarily organized to take care of the medical, nutritional, psychological, and social issues experienced by the patients.
The development of electronic information media such as dedicated websites is an essential part of addressing various issues and reaching people in remote places.
Future Trends and Institutional Commitment
As more and more people are undergoing bariatric surgical procedures these days, the demand for safe treatment facilities will grow. According to Dr. Atul NC Peters, Senior Consultant and Head of Apollo Institute of Metabolic and Bariatric Surgery, Indraprastha Apollo Hospitals, New Delhi, India, the most important element in the best bariatric surgery center is leadership from the surgeon and integrated medical staff. They require dedication, strong fundamental infrastructure, and total institutional commitment.