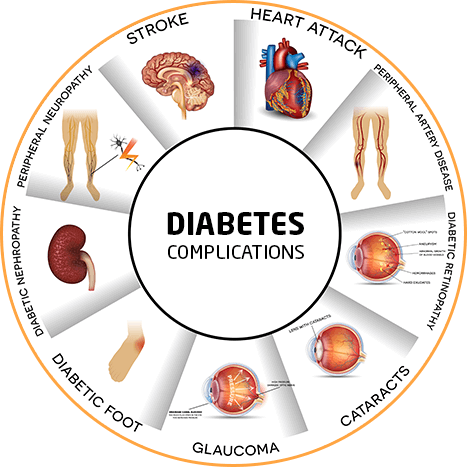
Diabetes is a chronic condition affecting millions globally. Type 2 diabetes is a metabolic disorder characterized by high blood sugar levels due to the body’s insulin resistance. It often develops over time due to lifestyle factors, obesity, and genetics, leading to serious health complications like heart disease, stroke, and kidney failure.
While lifestyle modifications and medications are the standard approaches for managing diabetes, some patients, particularly those with severe obesity and uncontrolled diabetes, may benefit from a more invasive treatment option like diabetes surgery, also known as metabolic surgery or bariatric surgery.
Obesity is increasingly identified as a major risk factor for type 2 diabetes. Understanding their complex relationship has become the dire need of the hour for effective prevention and management strategies.
Insulin Resistance: Obesity, especially visceral fat accumulation, can cause insulin resistance, making the body's cells less responsive to insulin. This leads the pancreas to produce more insulin, ultimately resulting in elevated blood sugar levels.
Inflammation: Excess body fat, especially around the abdomen, releases pro-inflammatory cytokines. These substances contribute to chronic low-grade inflammation, which is linked to the development of insulin resistance and type 2 diabetes
Hormonal Changes: Obesity alters the levels of various hormones which play essential roles in appetite regulation and metabolism. These hormonal changes can further disrupt insulin sensitivity and glucose metabolism.
Generally, lifestyle modifications and medications are the first steps to relieving the complications, but type 2 diabetes is a progressive condition that requires continuous care and treatment.
In situations like these, Metabolic/bariatric surgery is an immediate saviour that shows a rapid decline in blood sugar levels, reducing the need for diabetes medications and alleviating diabetes-related health problems.
Metabolic surgery refers to, a minimally invasive procedure that alters the stomach and intestine. It is an effective approach for treating obesity and health problems linked to type 2 diabetes.
Metabolic Surgery: A Dual Approach to Effective Blood Sugar Management
• First, weight loss - which is intended by the surgery - improves the body's ability to use insulin, especially on muscles and fat.
• Second, it directly impacts how the body reacts to food. It changes gut hormones, improves the functioning of the liver, and often benefits from better blood sugar levels even before significant weight loss.
Metabolic surgery targets specific metabolic processes, addressing the underlying causes of type 2 diabetes, which might lead to considerable improvement or even remission of the condition. While it is usually linked to weight loss, the approach goes beyond merely reducing food intake, it reduces one's risk of health complications developing in the future and improves overall quality of life.
• BMI above 32.5 kg/m2 with obesity-related co-morbidities
• BMI above 37.5 kg/m2 without co-morbidities
• BMI > 30 kg/m2 with life-threatening obesity-related disorders like uncontrolled diabetes, cardiovascular disease/cardiomyopathy, and severe obstructive sleep apnoea
• Patients motivated to lose weight and committed to long-term follow-up
• Patients should have attempted conservative methods of weight loss and fail in the past
• Metabolic surgery is to be considered only between the ages of 18 - 65 years
• Metabolic surgery may be considered in patients more than 65 years in the presence of severe obesity-related co-morbidities / disability
• Metabolic surgery may be considered in patients < 18 years in special situations after pediatrician/endocrinology certification, or after attainment of puberty or completion of skeletal maturity
To know if diabetes surgery is appropriate for you, consult your healthcare provider to discuss your potential benefits versus risks.
Metabolic surgery is an effective transformative intervention of the gastrointestinal tract offering a potent approach for sufferers of obesity and their comorbid conditions.
Alters the digestive tract.
• Reducing the Gut Capacity: Sleeve gastrectomy, a bariatric procedure, reduces the stomach's capacity. It leads to early satiety with minimized intake of food.
• Re-routing the Intestine: A part of the intestine is re-routed in bariatric procedures like gastric bypass surgery. Less calorie and nutrient intake are caused and act synergistically as a contributor to weight loss.
Provokes hormonal changes.
• Balancing Gut Hormones: Metabolic surgery alters hormones responsible for appetite, sensitivity, and glucose metabolism.
• Improving Insulin Sensitivity: Such hormonal changes can drastically enhance insulin sensitivity and reduce insulin resistance, which happens to be a major contributor to type 2 diabetes.
Limits calorie absorption.
• Nutrient Malabsorption: A part of the intestine is bypassed; gastric bypass surgery further worsens the nutrient and caloric absorption of food.
• Changes in Gut Microbiome: Malabsorption, in turn, causes gut microbiome imbalance that affects metabolic functions.
By altering the digestive system, these procedures promote significant weight loss and induce beneficial metabolic changes, leading to improved blood sugar control.
“Metabolic surgery for diabetes in India” offers a promising opportunity for people with type 2 diabetes, giving an option for disease management for which many have been waiting.
Key Benefits:
• Substantial Weight Loss: Prolonged weight loss is possible with metabolic surgery, thus reducing the risk of obesity-related co-morbidities and improving health.
• Improved Glycemic Control: Metabolic surgery supports remission of type 2 diabetes. It acts by improving the body's sensitivity and responsiveness to insulin.
• Lower Rate of Complications: Metabolic surgery reduces the rate of complications brought about by obesity and diabetes, some of which are heart diseases, stroke, and kidney-related diseases.
• Improved Overall Quality of Life: Surgery ultimately helps people feel more energetic by managing obesity and its associated complications, thereby boosting self-esteem and overall well-being.
By understanding these benefits, individuals can make informed decisions about their health and explore diabetes surgery as a viable option for managing their condition.
However, candidates for diabetes surgery must be committed to long-term lifestyle modifications to maximize the benefits of this transformative procedure.
Dr. Atul N.C. Peters is one of the leading bariatric surgeons. Having spent more than two decades in this field, he established the Department of Bariatric, Minimal Access, and Robotic Surgery at Max Smart Super Speciality Hospital, Saket, Delhi, India as a center of excellence.
Metabolic surgery has proven to be a powerful intervention not only to manage type 2 diabetes but even to 'cure' the disease. The most recent studies amply show how, for 80% of the patients, complete remission of the disease is achieved after surgery. For the remaining 20%, metabolic surgery greatly improves their condition, reducing medication intake and the use of injectable insulin.
It is noteworthy that metabolic surgery must only be conducted in specialized centers by experienced, specifically trained surgeons to ensure maximum benefits and fewer complications associated with the surgical procedure.
Dr. Peters is a recognized figure around the world in the medical field for his professionalism, commitment to care, and dedication toward his patients. He is acknowledged as a "Surgeon of Excellence" by the Surgical Review Corporation. He is established as a prominent leader in this specialty for performing successful metabolic surgery for diabetes in India.
With advanced medical infrastructure and promising quality of services, diabetes surgery in Delhi can be an effective solution for many!
• State-of-the-Art Hospitals: Delhi is home to many world-class hospitals equipped with the latest medical technology and facilities, ensuring that diabetic patients receive high-quality medical care services.
• Specialized Centers: Delhi has specialized, accredited centers with comprehensive treatment.
• Renowned Surgeons: Delhi boasts internationally renowned surgeons specializing in diabetes surgery, who have treated thousands of patients, globally, with very high success rates.
• Personalized Treatment Programs: There are expert surgeons here, who will design your treatment plan keeping your requirements as a patient in mind.
• Multi-specialty Teams: Most private hospitals in the city have multidisciplinary teams consisting of endocrinology, nutrition, and psychological experts, who will collaborate to offer holistic care for diabetes patients.
• Surgical Support Post-Ops: Comprehensive post-surgical care ensures optimal recovery and effective long-term management of diabetes following treatment.
Therefore, with specialist surgeons for ‘diabetes surgery in Delhi,’, advanced health infrastructure and a holistic approach to care, enhance the quality of life and well-being of patients.
Mr Narendra Pal Singh was obese with a BMI of 45.5 and was suffering from diabetes, high blood pressure, and sleep apnea.
Post his "diabetes surgery in Delhi", undertaken in 2013, the patient Mr. Singh’s health significantly improved. In 18 months, his blood sugar levels fell dramatically as the HbA1c from 8.0 to 6.3, making him stop his medications for both his diabetes and high blood pressure. Today, he maintains a healthy weight and a BMI of 33.4.
The cost of surgery for ‘diabetes surgery in Delhi’ will differ, but getting a gist of what influences the price range of this line of treatment is imperative and will go a long way in making informed choices and helping you plan for it.
• Complexity of the Procedure: General cost depends on the technique used, the more invasive procedures, such as Roux-en-Y gastric bypass, might be costlier. On the contrary, less invasive procedures like sleeve gastrectomy may be less expensive.
• Hospital Choice: Private hospitals with better and more renowned facilities and surgeons might be costlier than government hospitals.
• Surgeon's Expertise: The greater the trained and experienced surgeons can charge; the higher fees entail compromises on skills as well as the quality of care.
• Pre and Postoperative Care: Pre- and post-operative consultations, tests, and medication add up in general.
• Insurance Coverage: Fortunately, your health insurance plan can cut back on the cost of treatment for diabetes out-of-pocket. However, coverage can be very different, so you should check your plan for specific details.
Though this expense would seem to run sky-high, one should put it into perspective with the long-run benefits of surgery and make an informed decision.
Preparations for the surgery hold various dimensions that shall play a vital role in bringing about a positive outcome. These include, among others, the following:
• Comprehensive diagnosis: Your physician must run a comprehensive check-up to determine your overall condition or fitness for the surgery. This may involve blood work and physical check-ups, or even a request for a meeting with other doctors or specialists.
• Dietary Changes: You may be put on a special diet prior to surgery to ensure your health is fully optimized in order to prevent complications associated with the surgery. This can be administered in the form of a reduction in eating some forms of food, such as sugary drinks or processed foods.
• Change in Medications: Some medications will have to be stopped or adjusted prior to surgery. Your doctor will guide you once your needs are evaluated.
• Quit Smoking: Quit smoking prior to surgery. Smoking may increase your risk of complications and also prolong your recovery process.
What to Expect During Your Recovery?
• Pain Management: Pain medication can help you begin to feel well as you heal. You are also likely to be on a liquid or soft diet for the first few weeks after surgery.
• Follow-up care: The various post-operative follow-ups with the operating surgeon and his or her team showcase their dedication to your care and recovery.
These recommendations from the surgeon’s end will prepare a patient well for diabetes surgery and contribute to overall success.
A healthy diet is essential for long-term success after diabetes surgery. Here’s a guide to post-surgery nutrition.
• Initial Recovery: Eat in small portions and have frequent meals, gradually increasing as your appetite improves. Limit sugary drinks, processed foods, and excessive simple carbohydrates in your diet.
• Weight Loss Phase: Focus your diet on mostly lean proteins, fruits, vegetables, and whole grains. Aim to limit unhealthy fats and processed foods.
• Maintenance Phase: Once you reach your goal weight, you can maintain a healthy diet to prevent regaining weight. It's important to take care of your portion sizes to avoid overeating.
• Supplements: Your doctor’s recommendation for specific supplements, could include vitamins and minerals, protein, or calcium with vitamin D.
• Pacing: Begin with light exercising. It could consist of walking. Gradually increase the duration of exercising and the intensity of the workout as your body heals.
• Strength Training: This helps minimize the loss of muscles and protect against loss of muscle mass.
• Regular Exercise: Be sure to attempt at least 30 minutes of moderate-intensity exercise most days of the week.
Aim for at least 30 minutes of moderate-intensity exercise on most days of the week.
By following these guidelines, you will make sustainable lifestyle changes that maximize the benefits of diabetes surgery and support long-term health and well-being.
Prof. (Dr.) Atul N. C. Peters is a well-known surgeon with over 25 years of experience. He is the Senior Director of Bariatric, Minimal Access, and Robotic Surgery and has made his department a global leader. Among others, Dr. Peters is reputed to perform the best ‘metabolic surgery for diabetes in India.’
As the Senior Director of Bariatric, Minimal Access, and Robotic Surgery, he has established his department as a global leader in the field. Dr. Peters is renowned for performing the finest metabolic surgery for diabetes in India, among other specialties.
Prof. Peters holds the record for performing the highest number of bariatric surgeries in one day. He is a Fellow in several important surgical groups and a Diplomate of the National Board (DNB). He has been instrumental in the start of the Asia-Pacific Chapter of the International Federation for the Surgery of Obesity and Metabolic Disorders (ACMOMS).
He played a key role in establishing the Asia-Pacific Chapter.
In addition to his surgical expertise, Prof. Peters is a certified fitness trainer and proficient in 18 different instruments.
Dr. Yogesh Gautam is an experienced surgeon with over 25 years of experience in the area, and currently is Associate Director and Advisor of the Department of Bariatric, Minimal Access & Robotic Surgery.
He graduated from Delhi University in 1978 and also earned a master's degree in surgery. In 1983, he became a Diplomate of the National Board of Surgery. He has trained more than 100 surgical students during his illustrious career.
Dr Gautam is a pioneer of Minimal Access Surgery in India and has been active in different teaching programs. He has worked in some of India's top-tier hospitals, including Sir Ganga Ram Hospital, Batra Hospital, and Max Hospital.
His contributions towards planning the Department of General and Laparoscopic Surgery, as well as its academic initiatives, in Kolmet Hospital are commendable. His expertise extends beyond surgery since he has an MBA in Healthcare from FMS, Delhi.
Dr. Atul Wadhwa is one of the most accomplished surgeons, well-versed in Bariatric, Minimal Access, and Robotic Surgery.
After his master's in surgery from the University of Rajasthan in the year 1999, he was a Registrar at Safdarjung Hospital where he achieved worthwhile experience. Under the able mentorship of Padmashree Dr. P.K. Chowbey, he further honed his skills with a fellowship program in Minimal Access Surgery at Sir Ganga Ram Hospital.
He has expertise in advanced laparoscopic surgery and has trained himself under the renowned Prof. Alferd Cuscheri Dundee, UK for Upper GI Laparoscopic Surgery. He has published extensively in international and national journals in the field and has been the recipient of the Best Paper Award. He has contributed his work in various chapters on Minimal Access Surgery.
Dr. Wadhwa is an active member of the national as well as international Association of Laparoscopic and Endoscopic Surgery and a frequent speaker at national conferences.
His interests include virtually every abdominal surgery from the minimally invasive to hepato-biliary, colo-rectal, and bariatric procedures.
With his training in the da Vinci robotic system, Dr. Wadhwa is an integral member of the robotic surgery team. Currently, he is a Principal Consultant in the Department of Bariatric, Minimal Access & Robotic Surgery.
Dr. Shalabh Agarwal is a known consultant in the field of Bariatric, Minimal Access, and Robotic Surgery. After having an adequate foundation in general and laparoscopic surgery during his residency training at Hindu Rao Hospital, Delhi, Dr. Agarwal pursues a career in surgical innovation with the latest minimally invasive techniques.
He has been professionally trained in chosen areas, not only in his home country but the world. This list includes a Bariatric & Metabolic Surgery Fellowship. Such training equips him to be able to assist with over 1000 bariatric surgeries. To name a few examples, he's been declared a winner by the International Bariatric Club for having successfully finished their advanced Bariatric Surgery course.
Besides possessing surgical skills, Dr. Agarwal is also an ACLS/BLS provider of the American Heart Association, and therefore, confirms his concern for patient safety. He is also exploring the data-driven approach of healthcare from the point of view of clinical outcomes monitoring and surgical audit.
He is also well-trained in hernia surgery, as he has completed a Fellowship in Hernia Surgery, FALS. He has also completed a master's course in Minimal Invasive Proctology from IMAST, Mumbai, and has also undergone training on the Da Vinci Robotic System.
Dr. Saurabh Goswami is a senior consultant at the Department of Bariatric, Minimal Access, and Robotic Surgery. She has been through a journey in medicine by first completing an MBBS degree at DYPMC, Pune, and further went on to do a master's in general surgery at BVP, Pune.
Besides, Dr. Goswami has enhanced her expertise with the prestigious fellowships of F.MAS, FALS, and FIAGES. She is an ACLS/BLS provider at the American Heart Institute, too.
Dr. Goswami has served in high positions in prestigious medical institutes. Some of them are PGIMSR ESI Hospital, Basaidarapur, and Max Smart Super Speciality, Saket. Her primary areas of interest include laparoscopic and advanced abdominal surgery, breast, and colorectal surgeries.
A well-trained individual in the Da Vinci Robotic System, Dr. Goswami is a great asset to the team of robotic surgeons. Her empathetic approach to patient care and exceptional surgical skills make her an object of veneration and love for most of them. She also runs specialized clinics focused on addressing women's surgical issues with personalized care and support.
Dr. Beena Arora, Chief Dietitian of the Department of Bariatric, Minimal Access, and Robotic Surgery is highly qualified with her master's in Nutrition and Dietetics and then her Ph.D. from the University of Delhi in Food and Nutrition. Most of her research work leaned towards how nutrition plays a critical role in bariatric surgery. The worth that Dr. Arora puts in experience rather than money has been collected after more than two decades of experience working with many hospitals and academic institutions.
Dr. Arora, as Chief Dietician, would be at the forefront of pre-operative assessment of nutritional status in bariatric patients, as well as post-operative care. Dr. Arora also manages the bariatric nutrition program directly, which includes helping to organize bariatric support groups. She provides a much-needed stabilizing influence and emotional and educational support to these patients.
Beyond her clinical role, Dr. Arora also oversees the nonsurgical weight loss program "Think Fit" and primarily bases her area of practice on nutrition support for patients who are prepared for intra-gastric ballooning. She continues to contribute to the advancement of patient care through involvement in bariatric data management and research to help continue to enhance evidence-based practices.
An active educator, Dr. Arora spreads expertise through social media and blogging. She is a faculty member of the CICO (Certification in Integrated Care of Obesity) program, run jointly by OSSI and IFSO. She is a member of several professional bodies including IDA, OSSI, ADE, and IAPEN.
Ms. Nalini Massey has been an asset to the Department of Bariatric, Minimal Access & Robotic Surgery, having served the establishment for more than 14 years as a Program Manager. She acts as an interface between the patients and the coordinator; she organizes workshops, CMEs, and all kinds of marketing and academic activities.
Ms. Massey is in charge of the coordination of the operation theatre, admission, finance, operations, and inpatient services to be directed so that everything inside the institute works well, including the management of patients according to the schedule.
Another of the main expertise areas that Ms. Nalini has coordinated with international patients. In addition to taking care of the patients' travel and accommodation arrangements, she makes sure that their treatment goes on as hassle-free as possible. It is her dedication and commitment to the mission that can easily make otherwise complex tasks more manageable and provide exceptional services.