While conventional Bariatric surgery treats diabetes in obese patients some procedures like ileal interposition specifically treat diabetes even in patient who are otherwise not overweight.
The laparoscopic Ileal-Interposition with SG is a promising procedure for control of type 2 diabetes mellitus, hypertension, weight reduction, and associated metabolic abnormalities.
Ileal interposition is a novel operation first originated in Brazil for the treatment of type II diabetes. It was First presented by the Brazilian surgeon Aureo De Paula in 1999.
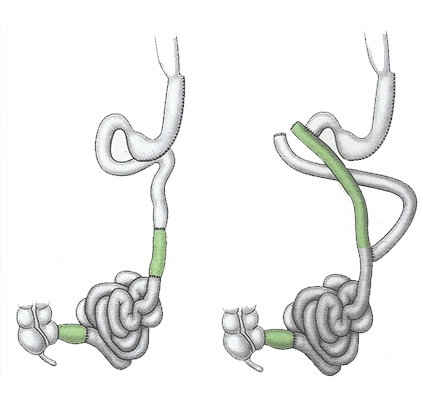
This surgery involves reducing the size of the stomach by doing a sleeve gastrectomy and in addition a distal or final segment of small intestine (ileum) is brought forward and connected to the initial or flexible small intestine (duodenum). Each surgical step in ileal interposition procedure is intended to have a hormonal target.
Position of patient is different in this because this surgery involves operation in the lower part of abdomen as well. So a patient is placed in supine position after general anesthesia.
A sleeve gastrectomy is performed in standard manner. In non-obese patients a relatively lose sleeve is performed so that there is less restriction of food intake.
The procedure begins with creation of a 170 cm segment of ileum(last part of small intestine) and interposition it into jejunum ( middle part of small intestine). There are three anastomoses or joints which may be done with staplers or suturing.
There are certain hormones which increases the sensitivity of insulin like GLP-1 and certain insulin resistance hormones like ghrelin, GIP, glucagon which are secreted normally in our gastrointestinal tract. The Aim of ileal interposition is to increase the insulin sensitivity hormones and to leave the resistance hormones aside.
Diabetes control is good following surgery, patients showing more than 80% reduction in diabetes drug requirement. Hypertension improves in more than (90%) patients. There is significant reduction in microalbuminuria postoperatively.
Recent studies have confirmed that II with SG is effective even in non-obese diabetic patients with BMI of 23–34 kg/m2 to improve their glycemic and metabolic derangement. The key strengths of these studies are the safety and efficacy of the surgery in treating patients with T2DM with a lower BMI and metabolic improvement beyond glycemic control.
They showed sustained glycemic improvement with preservation of beta cell function (pancreatic function) and cardiovascular benefits.