First open gastric bypass was described by Mason and Ito in 1966. The gastric bypass was based on the weight loss observed among patients undergoing partial stomach removal for ulcers. Over several years, the gastric bypass has been modified into its current form, using a Roux-en-Y limb of intestine (RYGB). The RYGB is one of the most commonly performed operation for weight loss all over the world.
The First laparoscopic gastric bypass was performed by Wittgrove and Clark in 1994.
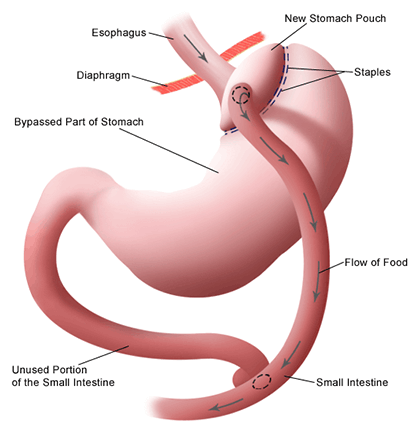
Roux-en-Y Gastric bypass surgery is an operation in which a small pouch of stomach is created and joined to the small intestine after bypassing an initial segment of small intestine known as duodenum and jejunum, thereby diversion of bile as well as intestinal secretions.
Aim of this arrangement: To achieve long term weight loss with least side effects and complications. Leading to resolution of obesity and it's related comorbidities.
Preparation of patient before surgery: Every patient is evaluated by a team of experts before being taken for surgery which includes body composition analysis, dietary consults, evaluation by physician, pulmonologist, cardiologist and psychiatric evaluation. Some other expert evaluations are done on case to case basis. There is mandatory thromboembolism prophylaxis 6 to 12 hours before surgery with antibiotics if needed.
Positioning of the patient in operation threatre: In the operation theatre, patient is placed in a special position called reverse Trendelenberg’s position after general anesthesia.
Operating Ports: There are usually 3 to 4 small operating incisions, which in 99 % cases don’t have any stiches or bandages post operatively. These are usually closed by special glue so that patient can have bath after the surgery. There are no pipes in most of the cases.
Formation of small gastric pouch: First step is formation of a small gastric pouch by use of surgical staplers. The pouch is formed on a special tube called a gastric caliberation tube.
Bypass: About 100 to 170 cm of the small intestine is bypassed
The intestines are re-attached to the stomach pouch by various mechanisms, like stapler or by suturing.
The net effect of this re-arrangement is a restricted intake of food; and due to the bypass, some malabsorption also takes place, leading to weight loss and resolution of Diabetes. However it is not only the restriction and malabsorption that leads to weight loss and correction of co-morbidities in obese people. The intestine in our body secretes a number of hormones, which are increased when exposed to undigested food. These hormones modify the metabolism in our body in such a way that diabetes is either resolved or controlled. Similarly blood pressure and a host of other problems are corrected due to these hormonal changes. Some of these hormones also increase our resting metabolic rate such that we consume more energy even at rest.
After surgery, there are sometimes marked changes in behavior. There is reduction in hunger as well as early satiety after small meals. These complex behavioral changes are partially due to alterations in several hormones (ghrelin, GIP, GLP, PYY) and neural signals produced in the GI tract that communicate with the hunger centers in the brain.
Many studies done at Center of Excellence in bariatric surgery all over the world report about 80% of excess weight loss after roux-en-y gastric bypass. Weight loss is achieved over a period of 18 months from the day of surgery and depends on various factors from patient to patient.
The obesity-related comorbidities that may be improved or cured with the RYGB include type 2 diabetes mellitus, high blood pressure, high cholesterol, arthritis, urinary stress incontinence, liver disease, certain types of headaches, heartburn, obstructive sleep apnea and many other disorders.
RYGB has also resulted in marked improvements in quality of life.